Have you been trying to conceive without success, feeling the weight of each passing month? You’re not alone, and understanding the underlying causes can be the first step toward a solution. One potential issue might be blocked fallopian tubes—a common but often undiscussed barrier to natural conception. Let’s explore how fallopian tubes work, what causes them to become blocked, and the steps you can take to achieve your dream of parenthood.
The Role of Fallopian Tubes in Fertility
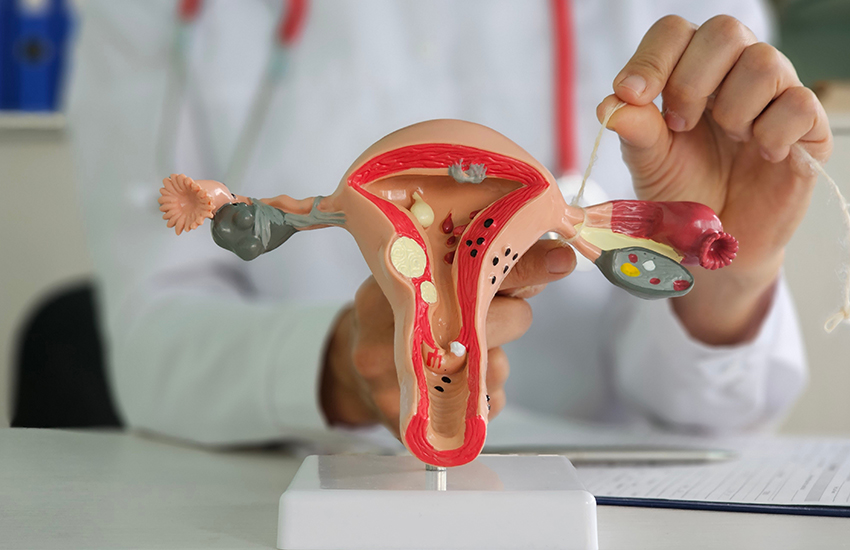
Fallopian tubes are essential players in the journey to conception. Each month, during ovulation, an egg is released from the ovary into the nearest fallopian tube. This is where fertilization occurs if sperm are present. The fertilized egg then travels through the tube to the uterus, where it implants and grows into a pregnancy. Open and functional fallopian tubes are thus crucial for natural conception. Any blockage or damage can prevent the egg and sperm from meeting, creating a significant hurdle in the fertility journey.
Common Causes of Blocked Fallopian Tubes
Several factors can lead to blocked fallopian tubes, affecting their ability to facilitate conception:
-
Infections and PID
Sexually transmitted infections like gonorrhea and chlamydia are common culprits. If untreated, these infections can lead to pelvic inflammatory disease (PID), causing inflammation and scarring that block the fallopian tubes. This scarring disrupts the smooth passage of the egg and sperm, making natural conception difficult.
-
Past Surgeries
Surgeries related to the reproductive organs, such as those for endometriosis or uterine fibroids, can inadvertently damage the fallopian tubes. Scar tissue from these surgeries can block or narrow the tubes, impacting their function.
-
Endometriosis
Endometriosis occurs when tissue similar to the lining inside the uterus grows outside it, including on the fallopian tubes. This can cause blockages or adhesions that hinder the egg’s journey to the uterus. It’s a common condition that can severely impact fertility.
-
Ectopic Pregnancy
An ectopic pregnancy, where a fertilized egg implants outside the uterus, often in a fallopian tube, can cause significant damage to the tube. This damage can lead to scarring and blockages, preventing future pregnancies from occurring naturally.
-
Tubal Ligation
Tubal ligation is a surgical procedure for permanent contraception, involving the cutting or sealing of the fallopian tubes. While it is intended to be permanent, some women may seek reversal, which isn’t always successful and can leave the tubes partially or fully blocked.
Read more: Understanding the Root Causes of Infertility
Symptoms and Diagnosis
Interestingly, many women with blocked fallopian tubes experience no symptoms, making the condition difficult to identify without medical intervention. Diagnosis often involves several procedures:
-
Hysterosalpingography (HSG)
HSG is an X-ray procedure where a dye is injected into the uterus and fallopian tubes. This dye helps to visualize blockages, providing a clear picture of whether the tubes are open or blocked.
-
Sonohysterography
This procedure involves injecting saline into the uterus and using ultrasound to detect abnormalities. It’s less invasive and provides valuable information about the condition of the fallopian tubes.
-
Laparoscopy
A laparoscopic procedure involves inserting a small camera through an incision in the abdomen to directly visualize the fallopian tubes and surrounding organs. It’s highly effective for diagnosing and sometimes treating blockages.
-
Hysteroscopy
Hysteroscopy involves examining the inside of the uterus and the openings of the fallopian tubes using a thin, lighted tube. It’s useful for detecting and addressing abnormalities within the uterus that might affect the fallopian tubes.
Treatment Options
Treatment for blocked fallopian tubes depends on the severity and location of the blockage. Several strategies are available:
-
Tubal Cannulation
This minimally invasive procedure involves inserting a catheter through the cervix into the fallopian tubes to clear blockages. It’s often successful for proximal blockages near the uterus.
-
Salpingectomy
In cases where the fallopian tubes are severely damaged, a salpingectomy, or removal of the tubes, may be recommended. This can be a precursor to IVF, ensuring no ectopic pregnancies occur.
-
In Vitro Fertilization (IVF)
IVF bypasses the fallopian tubes entirely. Eggs are retrieved from the ovaries and fertilized in a laboratory, with the resulting embryos implanted directly into the uterus. IVF is a common and effective treatment for those with blocked fallopian tubes.
Moving Forward with Treatment
If you suspect you have blocked fallopian tubes, seeking a fertility evaluation with a specialist is crucial. Personalized treatment plans based on individual fertility assessments can make a significant difference. Each woman’s situation is unique, and working closely with a specialist ensures the most effective treatment approach.
Conclusion
While blocked fallopian tubes present a significant hurdle, they do not mark the end of the road for aspiring parents. With modern medical advancements and personalized treatment plans, many women overcome this challenge and achieve successful pregnancies. Explore all available options, maintain hope, and take proactive steps toward your dream of parenthood with Fyne IVF.
Blocked fallopian tubes are just one of many hurdles on the path to parenthood, but with the right support and treatment, you can find your way forward. Stay hopeful and informed, and remember, you are not alone on this journey.