In vitro fertilisation (IVF) is a complex and meticulous process designed to help individuals and couples conceive a child. It becomes imperative to understand the various stages of embryo development, as this knowledge often raises important questions and holds vital implications for IVF success.
One of the critical stages in this process is the development and transfer of the blastocyst, which holds great significance for IVF success. This blog delves into understanding blastocysts and how they influence fertility and treatment outcomes.
What is a Blastocyst?
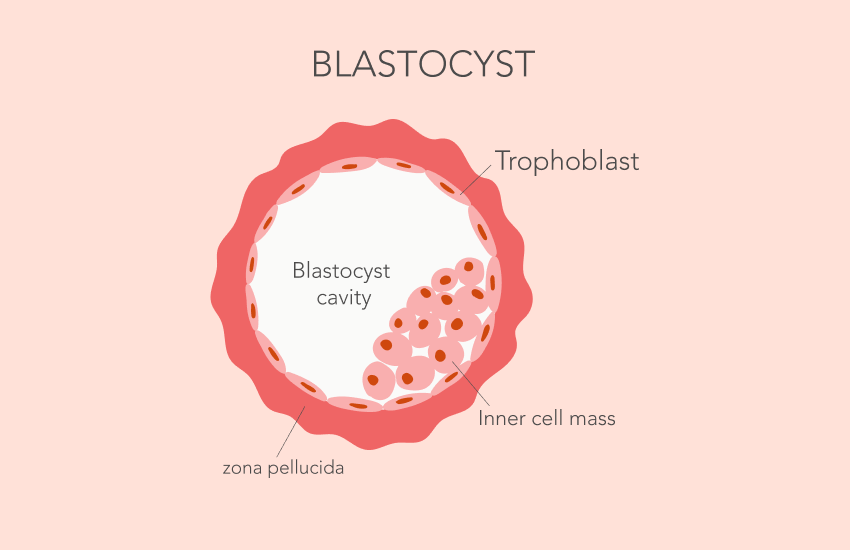
Blastocysts are early-stage embryos that form after fertilisation. They develop from a zygote, which is a single cell resulting from the fusion of a sperm and an egg. A blastocyst has two distinct cell types and a central cavity filled with fluid. The outer cell layer, called the trophoblast, will eventually form the placenta, which is essential for nourishing the embryo throughout pregnancy. The inner cell mass (ICM) will develop into the foetus itself.
Blastocyst Development Stages
The development of a blastocyst occurs over a few key stages:
1. Zygote (Day 1): This is the single-cell stage, immediately following the fertilisation of the egg by the sperm. The zygote contains genetic material from both parents.
2. Cleavage stage (Days 2-3): The zygote begins to divide, forming a multicellular structure.
3. Morula (Day 4): By the fourth day after fertilisation, the embryo becomes a solid ball of cells, known as a morula.
4. Early blastocyst (Day 5): Around the fifth day, the morula transforms into a blastocyst. The cells of the outer layer (trophoblast) begin to form a sphere, while the inner cell mass clusters on one side of the blastocyst.
5. Expanded blastocyst (Day 6): At this stage, the blastocyst becomes larger, and the cavity inside the blastocyst (blastocoel) expands, pushing the inner cell mass and trophoblast further apart. This prepares the blastocyst for the next phase of implantation in the uterine lining.
6. Hatching blastocyst (Day 6-7): For implantation to occur, the blastocyst must break free from the zona pellucida, a protein membrane surrounding it. This is known as ‘hatching’. Once free, the blastocyst is ready to attach to the uterine wall and begin the process of implantation.
Blastocyst Quality and Grading
Not all blastocysts are created equal and embryologists assess blastocyst quality using a grading system. The grading is based on three criteria: the expansion of the blastocyst cavity, the appearance of the inner cell mass, and the quality of the trophoblast cells.
The stages of blastocyst embryo development are divided into four grades, namely:
Grade 1: The embryo with a blastocoel cavity less than 50% of the embryo volume.
Grade 2: The embryo with a blastocoel cavity as much as 50% of the embryo volume or more.
Grade 3: The blastocoel cavity has expanded, and the zona pellucida (ZP) appears thinner than the embryo at day 3.
Grade 4: Embryo that has successfully hatched from ZP.
Research has shown that higher-quality blastocysts (e.g., a 5AA blastocyst-where ‘5’ refers to day 5 of development, and ‘A’ grades are given for both the inner cell mass (ICM) and the trophectoderm (TE)) correlate with better reproductive outcomes, including higher live birth rates and lower miscarriage rates.
Why the Blastocyst Stage is Important in IVF
In natural conception, only a small percentage of embryos make it to the blastocyst stage and successfully implant in the uterus. There are several reasons why transferring a blastocyst during IVF is advantageous over transferring an earlier-stage embryo:
1. Higher implantation rate: The embryo is more developed at the blastocyst stage, which means it is closer to the point of implantation.
2. Better embryo selection: By allowing embryos to develop to the blastocyst stage, embryologists can better assess their quality.
3. Synchronisation with the uterine environment: The blastocyst stage aligns more closely with the natural timing of implantation. In a natural cycle, embryos typically reach the uterus and implant around the fifth or sixth day after fertilisation.
4. Single embryo transfer: Because of the higher implantation rates associated with blastocyst transfers, there is less need to transfer multiple embryos.
What are the Challenges and Considerations here?
While the blastocyst stage offers numerous benefits, there are challenges associated with blastocyst transfer. Not all embryos reach this stage, and some may exhibit chromosomal abnormalities that can lead to implantation failure or miscarriage.
There is also a risk that no embryos will reach the blastocyst stage, leaving no viable embryos for transfer. Therefore, careful screening and grading of embryos are essential to optimise outcomes in IVF treatments.
The blastocyst stage represents a pivotal moment in embryonic development, significantly increasing the success rate of IVF due to better embryo selection, genomic activation, and endometrial receptivity, thereby influencing fertility treatment outcomes. By allowing embryos to reach this advanced stage before transfer, fertility specialists can enhance the chances of successful implantation and healthy pregnancies.
For those considering IVF, it is essential to consult with experienced professionals who can guide you through the process, ensuring that you receive personalised care tailored to your unique needs.
Fyne IVF is dedicated to providing comprehensive support and advanced reproductive technologies to help you achieve your dream of parenthood.
FAQs – Understanding Blastocysts in IVF
1. What is a blastocyst in IVF?
A blastocyst is an early-stage embryo that forms around five to six days after fertilization. It has two distinct cell types and a fluid-filled cavity and is more likely to implant successfully during IVF.
2. Why is the blastocyst stage important in IVF treatment?
Transferring a blastocyst increases the chances of implantation, allows for better embryo selection, and aligns more closely with the natural timing of implantation.
3. What are the stages of blastocyst development?
Blastocyst development progresses through several stages: zygote (Day 1), cleavage stage (Days 2–3), morula (Day 4), early blastocyst (Day 5), expanded blastocyst (Day 6), and hatching blastocyst (Days 6–7).
4. How is blastocyst quality graded?
Blastocysts are graded based on cavity expansion, the quality of the inner cell mass, and the appearance of the trophoblast. Higher-grade blastocysts are linked to better IVF outcomes.
5. What are the benefits of transferring a blastocyst instead of a Day 3 embryo?
Blastocyst transfer offers higher implantation rates, better embryo selection, and reduced need for multiple embryo transfers, thus minimizing the risk of multiple pregnancies.
6. Are there any risks or challenges with blastocyst transfer?
Yes. Not all embryos reach the blastocyst stage, and some may have chromosomal issues. In some cases, there may be no blastocysts suitable for transfer, requiring careful monitoring and planning.